Client adherence to treatment for type 2 diabetes, obesity, and other chronic health problems is a great source of concern for physicians. Physicians often look to mental and behavioral health professionals to help care for their clients with chronic illnesses, while grappling with how to increase adherence to treatment.
What are the possible obstacles clients face?
- The complexity of treatment can influence adherence.
- There may be unpleasant or intolerable side effects from medication.
- The proposed changes in lifestyle may seem impossible to the client.
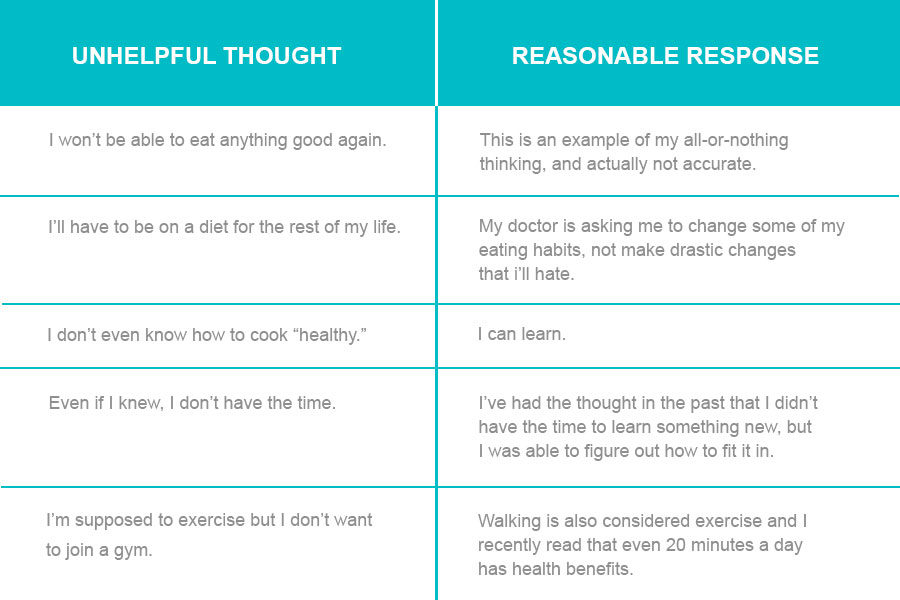
- The client may be engaging in cognitive distortions such as dichotomous thinking or catastrophic thinking.
Many life-long health problems require the client adopt a self-management approach to regulate the course and impact of the problem, but clients often lack the necessary skills or engage in problematic thinking. Changes in self-care, including adjustments in eating behavior, can lead clients to experience frustration and helplessness, and adherence to a medication protocol can be challenging or off-putting to clients.

It has long been understood that lifestyle choices are associated with health as well as disease and mortality. In a study by King, Mainous, and Everett (2009), adherence to a healthy lifestyle pattern decreased in the 18 years studied, while evidence of declining health increased. Similarly, findings by Ford, Bergman, Boeing, Li and Capewell (2012) suggest that adults who consume a healthy diet and engage in sufficient physical activity can significantly reduce their risk for early death. In a diverse sample of adults ranging in age from 45 -64, King, Mainous, and Geesey (2007) found that people who only adopted a healthy lifestyle in middle-age, experienced an immediate benefit of lower rates of cardiovascular disease and mortality. This study gives hope that even after decades of poor lifestyle habits, concomitant poor health can change.
Changing lifestyle habits is often experienced as difficult by clients, making goal-setting and treatment planning challenging. Typical questions such as, “What would you like to change about the problem you described to me?” or “What would you be doing more of and what would you be doing less of as the result of therapy?” are not necessarily helpful if the client feels overwhelmed or helpless.
Consider the example of Joanie, a 64-year-old female who came to see me upon the suggestion of her primary care physician. Joanie was pleasant, but confused as to why her doctor wanted her to see a psychologist; after all, she felt fine. She was having trouble managing her blood glucose levels though, and felt unable to make the changes her doctor prescribed. I began by explaining to Joanie that she and I could work together to discover what the obstacles were and collaboratively, we could come up with solutions. I used the information I gleaned from the cognitive case conceptualization, and understood that Joanie’s helplessness core belief was triggered when her physician asked her to make lifestyle changes she didn’t think she was capable of. Once I understood what Joanie was thinking, then how she was feeling and what she was doing (and not doing) made perfect sense. After I taught Joanie to identify negative and unhelpful automatic thoughts, we worked on modifying her responses to be more adaptive and reasonable.
The way clients respond to the challenges of preventing and managing chronic illness is of particular interest to cognitive behavioral clinicians, as we have the tools to help patients modify thinking and behavior to improve health and quality of life.
References
Ford, S. F., Bergman, M. M., Boeing, H., Li, C., & Capewell, S. (2012). Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Preventive Medicine 55 (1), 23-27.
King, D.E., Mainous, A.G., & Everett, C. J (2009). Adherence to healthy lifestyle habits in US adults, 1988-2006. The American Journal of medicine, 122(6); 528-534.
King, D. E., Mainous, A. G., & Geesey, M.E. (2007). Turning back the clock: adopting a healthy lifestyle in middle age (2007). The American Journal of Medicine, 120(7), 598-603.